IUI
Intrauterine Insemination or IUI is sometimes also called Artificial Insemination or AI. The reason your fertility specialist may discuss it as a potential choice for your fertility treatment, may be linked to poor ovulation, or to your partner’s sperm quality.
Other reasons to explore IUI can be linked to your relationship status: in case you are a single woman, or if you are a female same-sex couple, then IUI might be one of the options your specialist will discuss with you. Please note that on our website, the Fertility Society is not providing any medical advice, and that it is important to obtain customised and personalised advice from your local qualified fertility specialist.
What is IUI?
Intrauterine Insemination in simple words is inserting sperm into the uterus. This is done in a procedure at your fertility clinic. Before the insemination, your partner’s sperm is washed and prepared, and the most motile sperm is isolated to be inserted.
IUI is often combined with a procedure to influence the woman’s ovulation, in a process we call ovarian stimulation. With intrauterine insemination it is critical to apply a strict timeline and to know exactly when the prepared sperm is to be inserted into the uterus. Using ovarian stimulation may give the specialist more parameters to influence, to increase a couple’s chances to fall pregnant.
To define if IUI is the right type of assisted reproductive technology (or fertility treatment) for you and your partner, speak to your local qualified specialist. The choice of treatment will depend on your fertility history, your partner’s fertility and medical history.
This is an overview of a typical intrauterine insemination process. Please note that all decisions about steps in your personal treatment will be taken by your qualified fertility specialist and that this information is not to be used as medical advice.
Step 1: Ovulation induction
As a woman, you are prescribed hormone treatment, either as oral medication or in the form of daily injections that you will administer yourself. The drugs optimise your cycle and they stimulate your ovulation.Step 2: Semen sample
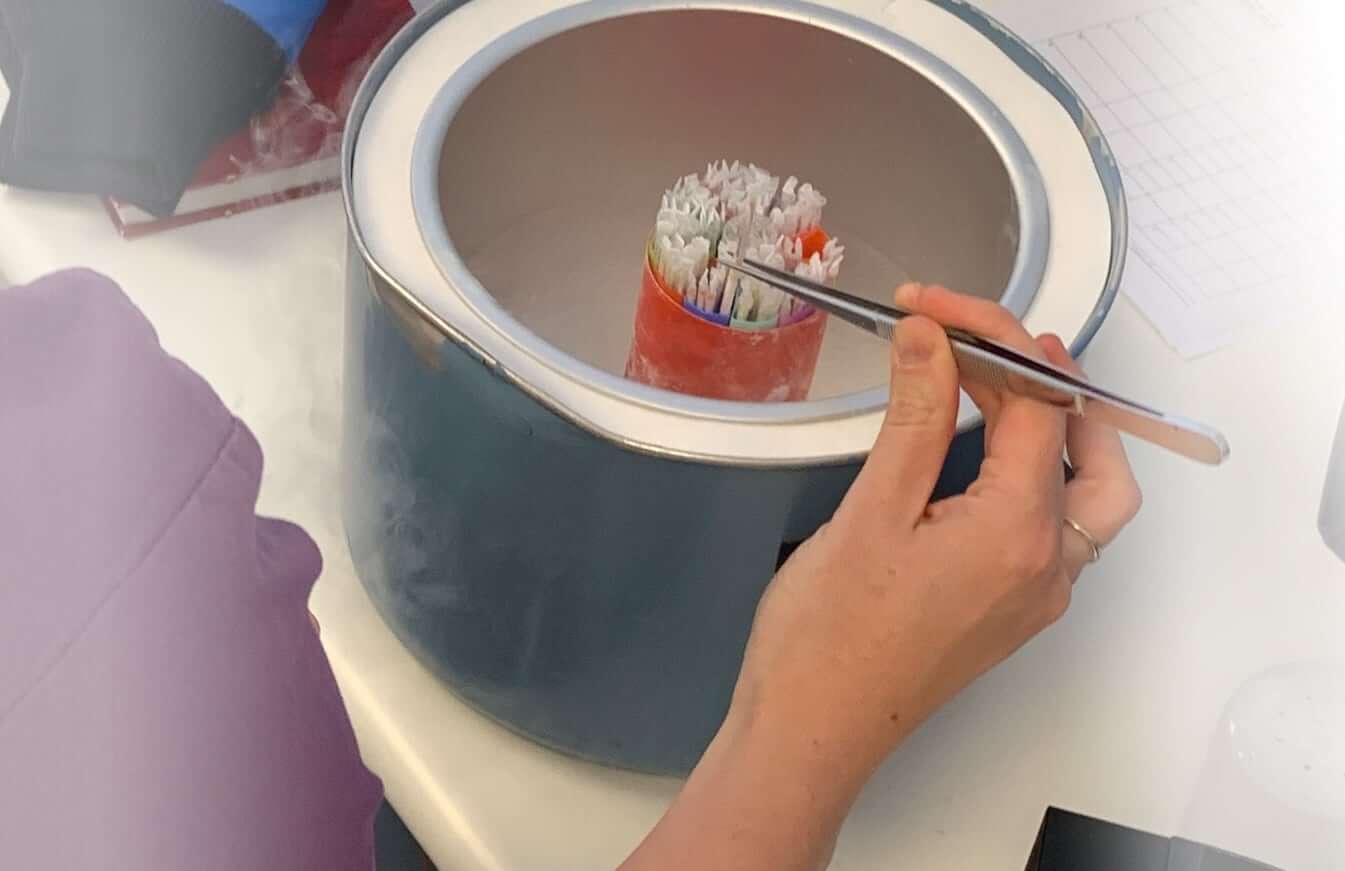
At the fertility clinic, the man’s semen sample is collected and analysed. The process includes the selection of the most optimal sperm in terms of strength and motility. The concentrated semen sample is then prepared for the artificial insemination.Step 3: The insemination
The procedure is timed depending on your cycle, and usually is not experienced as painful. On the day of the procedure, the prepared semen is inserted into your uterine cavity. Your specialist will prescribe progesterone to support the final stage of your cycle.Step 4: Pregnancy test
At a time indicated by our specialist, you will perform a pregnancy (blood) test.IUI is recommended - and will be discussed as one of the options when you consult your qualified fertility specialist or fertility clinic - in a number of different situations:
- Unexplained infertility:
You have trouble falling pregnant Artificial insemination is often the recommended fertility treatment if as a couple you suffer from unexplained fertility. There can be a number of problems that prevent sperm from passing through the cervix into your uterus, and some of the problems can be related to poor cervical mucus or age. What IUI does is bypassing this stage, with a direct insert of sperm into your uterus. Reduced sperm motility or poor cervical mucus are then no longer an obstacle.
- Absence of the male partner:
Partner is not in the same location or is scheduled to undergo cancer treatment. In this case, the artificial insemination procedure makes use of thawed sperm that was frozen at an earlier stage. The insemination is scheduled when the female partner ovulates.
- Same sex couple or single woman trying to conceive:
Single women who want to have a child, would often explore IUI as the recommended approach. Same-sex couples (female) who wish to fall pregnant, will be able to use third-party sperm as part of their IUI procedure.
- Reduced sperm quality:
sperm count or motility less than ideal. If - as a male partner - you have slightly reduced sperm quality, then it can be hard to conceive. Your specialist will organise tests and assess if you suffer from reduced sperm count or reduced sperm motility. If the sperm quality shows really low numbers, or if there is a risk of transmitting a genetic disease onto your future children, then your specialist may discuss the option to explore conception with donor sperm.
IUI success rates
It is important to understand that the overall success rates of intrauterine insemination procedures are lower than the success rates of IVF. IUI has high rates of success when data from cumulative cycles are added up. In other words, when as a couple you start a new cycle when the previous cycle has failed. IUI is seen as less costly, and as a less invasive and emotionally less impactful procedure compared to IVF and ICSI.
Some studies refer to 60% of couples conceiving within six IUI cycles. Other data will claim that the overall pregnancy rates will not differ that much between IVF and IUI procedures. When looking at success rates, it is important to look at the way data has been collected. And even more important, it is important to speak to your specialist about your personal situation, and the pros and cons of IUI versus IVF.
0%
couples conceiving
0
IUI cycles
IUI risks
The main risk associated with IUI is the chance of multiple pregnancies. When IUI is used in conjunction with ovarian hyperstimulation, the woman being inseminated is likely to have a number of mature oocytes in her fallopian tubes at the time of insemination. Each of these has the potential to become fertilised if it comes into contact with a sperm and the chance of multiple pregnancy is therefore high. Multiple pregnancy carries greater health risks for the foetuses and the pregnant woman, including an increased risk of miscarriage and low birth weight and increased pressure on the body of the pregnant woman.
The treatment
Because ovarian stimulation may be used in combination with an IUI procedure, there is a risk of high numbers of mature oocytes in the fallopian tubes, known as ovarian hyperstimulation. If serious instances of OHSS (ovarian hyperstimulation syndrome) additional treatment in hospital may be needed.
The pregnancy
Because there is a higher likelihood of high number of mature eggs, the chance of
multiple pregnancy is high.
Children born from IUI
Because of a higher chance of multiple births, there is an increased risk of miscarriage and a risk of low birth weight. A multiple pregnancy also adds higher pressure levels on your body as a pregnant woman.
Donor sperm used in an IUI procedure will be sourced through an official donor programme.
In case of a male-factor infertility challenge, you can plan your treatment based on obtaining donor sperm from a family member or a friend. In this case, as a future intended mother, you would know the donor.
Alternatively, sperm donor programmes allow you to work with an agency and make use of sperm from a de-identified screened donor. It means that the sample has been thoroughly tested both for sperm quality, general health and genetic conditions. In this case you would not receive any information about the donor’s identity.
IUI combined with a sperm donor programme is a treatment avenue that can be discussed in case of poor sperm quality or the absence of sperm. Depending on the regulations that apply in your area, your specialist will explore the options to plan your treatment with a suitable donor.
Choosing a fertility clinic for IUI
The regulations that apply in your area are one factor to bear in mind when you choose your fertility clinic. We recommend that you verify your specialist’s qualifications and ask your GP to support you in the choice of your preferred specialist for fertility treatment.
Cost of IUI
IUI is generally less expensive than IVF or ICSI and can significantly reduce the overall cost of fertility treatment for many couples. For details about costs, ask your specialist about details in regards to the tests that you and your partner will need to undergo, as well as specific fees applicable for each step of the process.
References
- Helmerhorst FM, Van Vliet HAAM, Gornas T, Finken MJJ, Grimes DA. Intra-uterine insemination versus timed intercourse for cervical hostility in subfertile couples. Cochrane Database of Syst Rev 2005, Issue 4. Art. No.: CD002809
- Ombelet, W. Puttemans, P. Bosmans, E. “Intrauterine insemination: a first step in the algorithm of male subfertility” in Hum Reprod, 1995, 10(Supp 1):90-102.
- Abou-Setta, A.M. Mansour, R.T. Al-Inany, H.G. “Intrauterine Insemination Catheters for assisted reproduction: a systematic review and meta-analysis” in Hum Reprod, 2006, 21(8):1961-67.
- Dastur, A.E. “Artificial Insemination: Historical Review” in Intrauterine Insemination, ed. Gautem Allahbadia, 2005, Taylor and Francis, p 17-21.
- Miskry, T. Chapman, M. “The use of intrauterine insemination in Australia and New Zealand” in Hum Reprod, 2002, 17(4):956-959.